Contraception Options
Guide to Choose the Right Contraception
When deciding between a Combined Oral Contraceptive (COC) and a Progestogen-Only Pill (POP), key factors like your health, lifestyle, and personal preferences should be considered.
Combined Oral Contraceptive (COC)
- Highly effective (over 99% with perfect use).
- Can regulate periods, reduce menstrual cramps, and improve acne.
- Offers additional health benefits, such as reducing the risk of certain cancers (e.g., ovarian and endometrial cancer).
- You do not have a history of blood clots, heart disease, certain types of cancer (e.g., breast or liver cancer), or severe migraines with aura.
- You are comfortable with a daily pill and can take it consistently at the same time each day.
- Women who smoke AND are over 35.
- Women with a history of blood clots, stroke, heart disease, liver disease, or certain cancers (e.g., breast or liver cancer).
- Women with severe uncontrolled hypertension.


Progestogen-Only Pill (POP)
- Suitable for women who cannot take oestrogen, such as those with a history of blood clots or certain cancers.
- Can be used during breastfeeding without affecting milk production.
- No oestrogen-related side effects, like an increased risk of blood clots.
- You need a contraceptive method without oestrogen, particularly if you are breastfeeding or over 35 and smoke.
- You are able to take the pill at the same time every day, as timing is crucial for the effectiveness of the POP.
- Women with unexplained vaginal bleeding.
- Women with liver disease or certain types of liver disorders.
How to Decide

Consultation With a Healthcare Provider
It’s important to discuss your personal health history with a healthcare provider to help determine which method is most appropriate for you. They will guide you based on your health profile, preferences, and whether you have any contraindications for either method.
Alternative Contraceptive Options
Alternative contraception options are available through your GP or local sexual health service which are listed below:

Condoms
External (or male) condoms are thin coverings worn on the penis that act as a barrier to prevent sperm from reaching a partner during sex. They're suitable for oral, vaginal, and anal sex, and are the only type of contraception that also protects against sexually transmitted infections (STIs). There are also internal (female) condoms, which are worn inside the vagina.
When used properly, male condoms are 98% effective at preventing pregnancy. Female condoms are around 95% effective. They're free from hormones, so they don’t cause hormonal side effects.
You can get condoms for free from:
- Contraception clinics
- Sexual health clinics
- Some GP surgeries
- Some young people’s services
You can also buy them from:
- Pharmacies
- Supermarkets
- Online
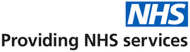
Contraceptive Implant
The implant is a small, flexible rod placed under the skin of your upper arm by a healthcare professional. It steadily releases the hormone progestogen to prevent pregnancy and lasts for up to three years. It can be removed at any time, and your fertility returns quickly afterwards.
Most women can have the implant. It’s ideal for those who don’t want to take a pill every day or who can’t use contraception with oestrogen. It might not be suitable if you:
- Take medicines that affect the implant
- Have or have had heart disease, stroke, liver disease, or breast cancer
Effectiveness: Over 99% effective.
Available for free at:
- Contraception clinics
- Sexual health clinics
- Some GP surgeries (check if yours offers it)

Contraceptive Injection
This method also uses progestogen to prevent pregnancy but is delivered via injection. Depending on the type, it lasts between 8 and 13 weeks. You’ll need repeat injections to stay protected.
Suitable for most women—especially those who can’t take oestrogen. It may not be right if you:
- Plan to get pregnant within the next year
- Have liver disease, osteoporosis, or a history of breast cancer, heart disease, or stroke
Effectiveness: More than 99% effective.
Available free from:
- Contraception clinics
- Sexual health clinics
- GP surgeries
Contraceptive Patch
A small sticky patch worn on the skin that releases oestrogen and progestogen to prevent pregnancy. You wear a new patch each week for three weeks, followed by a patch-free week.
Not suitable for everyone. You’ll need to discuss your medical history with a doctor or nurse. It may not be recommended if you:
- Are breastfeeding (baby under six weeks old)
- Are over 35 and smoke or recently quit
- Are overweight or have had breast cancer
- Take certain medications
Effectiveness: Over 99% when used correctly.
You can wear it while bathing, swimming, or exercising.
Available free from:
- Contraception clinics
- Sexual health clinics
- Some GP surgeries

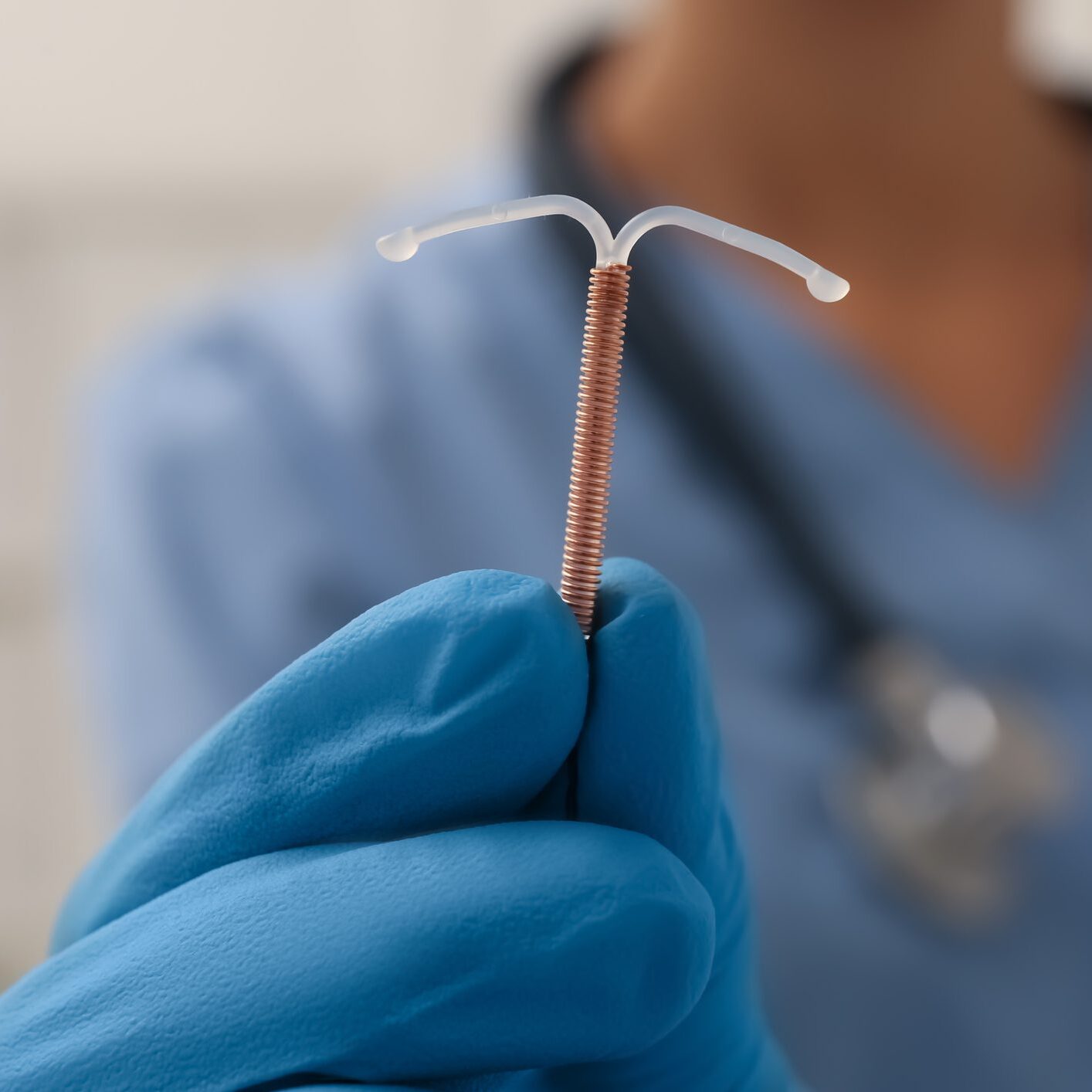
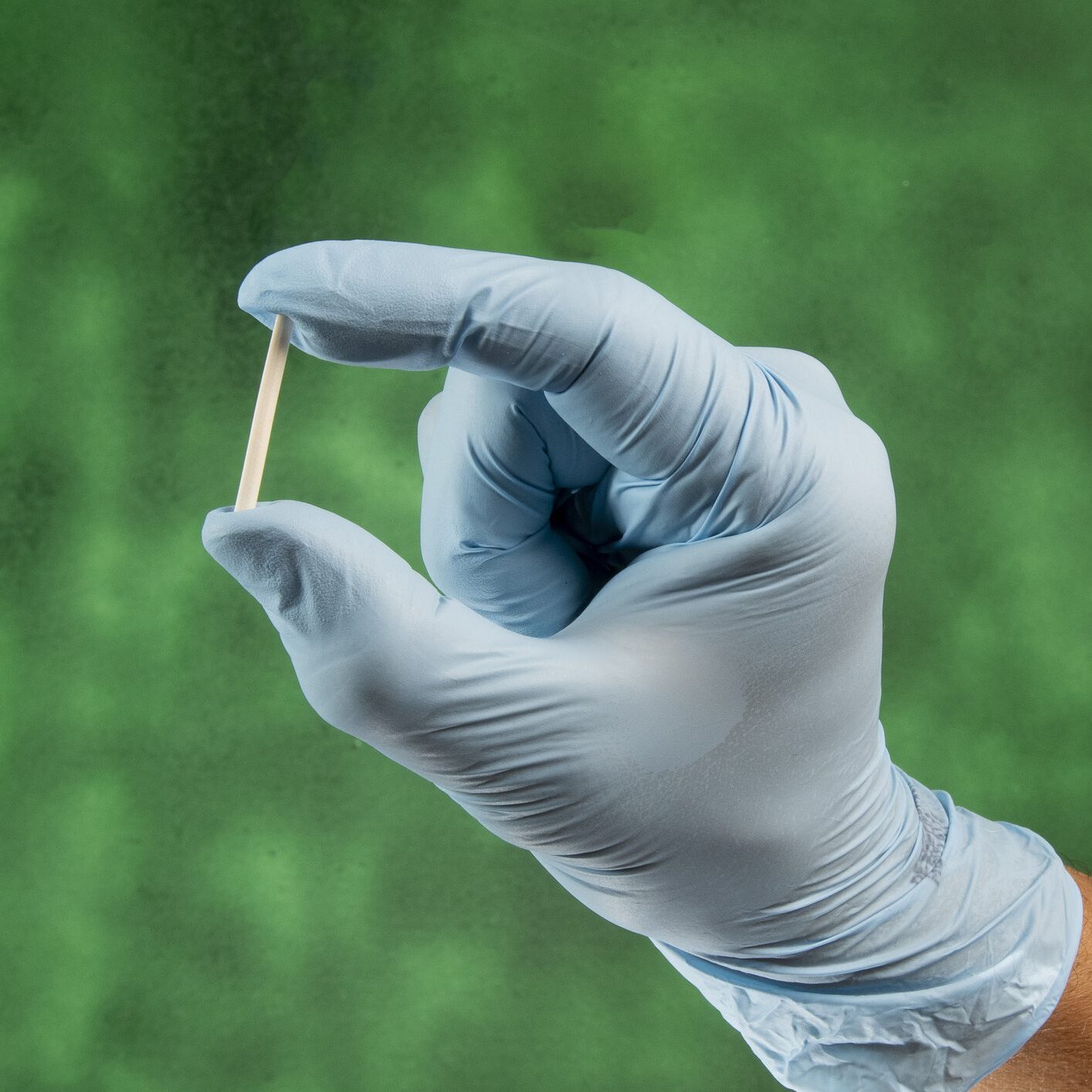
IUD (Intrauterine Device or Coil)
A small T-shaped device made of plastic and copper that’s inserted into the womb. It works immediately and lasts 5–10 years depending on the type.
Releases copper to prevent pregnancy by thickening cervical mucus and stopping a fertilised egg from implanting.
Most women can, especially those looking for a hormone-free option. It might not be suitable if you:
- Have an untreated STI or pelvic infection
- Have womb/cervix problems or unexplained bleeding
Effectiveness: Over 99%.
Available free from:
- Contraception clinics
- Sexual health clinics
- GP surgeries
IUS (Intrauterine System or Hormonal Coil)
Similar in shape to an IUD, but releases progestogen instead of copper. It thickens cervical mucus and can also stop ovulation. It lasts 3–5 years depending on the brand.
Most women can, though it may not be suitable if you:
- Have breast, cervical, or womb cancer
- Have liver or heart conditions
- Have an STI or unexplained bleeding
- Have womb/cervix issues
Effectiveness: Over 99%.
Available free from:
- Contraception clinics
- Sexual health clinics
- GP surgeries

Diaphragm or Cap
A dome-shaped piece of soft silicone placed inside the vagina before sex. It covers the cervix to prevent sperm from reaching the egg. Use it with spermicide.
Most women can, unless they:
- Have a differently shaped cervix
- Are allergic to latex or spermicide
- Have had toxic shock syndrome or frequent UTIs
- Have a current vaginal infection
Effectiveness: 92–96% when used correctly with spermicide.
Must be left in for at least 6 hours after sex.
Available from:
- Contraception clinics
- Sexual health clinics
- GP surgeries
Vaginal Ring
A soft plastic ring that’s inserted into the vagina and releases oestrogen and progestogen. Each ring lasts one month: wear it for 21 days, then take a 7-day break.
Not suitable if you:
- Have had blood clots, heart issues, or high blood pressure
- Are 35+ and smoke or recently quit
- Are overweight or had breast cancer
- Take certain medicines
Effectiveness: Over 99% if used correctly.
Available from:
- Contraception clinics
- Sexual health clinics
- GP surgeries
Note: Not all clinics stock the ring. You’ll only be given up to 4 months’ supply at a time due to its shelf life.


Natural Family Planning
This method involves tracking fertility signals daily—like cycle length, body temperature, and cervical mucus—to determine when you're most fertile.
Up to 99% if followed carefully and consistently. Less effective if not used precisely.
If you’re considering this option, make sure to learn from a qualified fertility awareness teacher.
Talk to your GP, nurse, or pharmacist to explore the best options for you. NHS contraception services are free and confidential, even for those under 16.